By Garry K. Smith
As presented at the 24th Biennial Conference of the Australian Speleological Federation, Jan 2003, Bunbury WA.
Also published in the proceedings.
Abstract
The terms “Pink Puffers” and “Blue Bloaters” have been around for many years. They are used in a colloquial sense by speleologists to describe how cavers react to an elevated concentration of carbon dioxide (CO2) and reduced oxygen (O2) in a cave’s “foul air” atmosphere. Foul air is only found in a small number of Australian caves and is defined as having a noticeable abnormal physiological effect on humans. Pink Puffers hyperventilate when exposed to foul air while Blue Bloaters are slow to react and run the risk of losing consciousness without warning.
This paper compares these colloquial terms with the same terminology used by some doctors to describe patients with medical conditions related to Chronic Obstructive Airways Disease (COAD). Pink Puffers hyperventilate and have good colour, while Blue Bloaters do not hyperventilate and look bluish because they are starved of oxygen. This is where the similarity in definitions ends. In the caving fraternity the term refers to a speleologist’s respiratory reaction to one of three types of foul air in a cave whereas in medical terminology it refers to a COAD patient’s specific condition and how their body functions in good air.
Also discussed are possible links between smokers and ex-smokers with early stages of COAD (not yet causing noticeable disability in good air) who go underground and when subjected to foul air become speleologist blue bloaters. Two possible scenarios are put forward for discussion, which could form the basis of a future research project for someone with access to lung function measurements equipment.
Introduction
The terms “Pink Puffer” and “Blue Bloater,” have been around for many years, but do we really know what they mean and how serious it can be for a person entering a cave containing the so called “foul air”? In the caving fraternity the terms are used colloquially to describe the physiological effect on a person exposed to foul air containing an elevated concentration of carbon dioxide (CO2) and reduced oxygen (O2). However, within the medical fraternity the terms are used to describe patients with medical conditions related to Chronic Obstructive Airways Disease (COAD). The meaning and use of these terms is examined in both a speleological and medical aspect. Also a possible link between smoking and the speleologist blue bloater is discussed.
What is foul air?
Foul air, sometimes called “Bad Air”, is an atmosphere which has a noticeable abnormal physiological effect on humans. (Smith 1999a). In limestone caves, foul air can be described as containing greater than 0.5% carbon dioxide (CO2) and/or lower than 18% oxygen (O2) by volume. As a comparison, normal air contains approximately 0.03% CO2 and 21% O2 by volume (Smith 1999b). Foul air is only present in a small number of caves around Australia. When encountered, it generally occurs as an elevated concentration of CO2 and a reduced concentration of O2. Either elevated CO2 or reduced O2 or a combination of the two can be life threatening (Smith 1997c). A high CO2 concentration is the most life threatening situation encountered underground while life threatening low O2 concentration is rarely encountered (Smith 1999b).
- Type 1 foul air results from the introduction of CO2 into the cave atmosphere and all other components mainly O2 and nitrogen (N2) are diluted - the source of the CO2 is immaterial.
- Type 2 foul air is the result of O2 being depleted and replaced with the CO2 by-product of organic and micro-organism metabolism or respiration by fauna such as bats or humans. In this instance the O2 concentration is reduced in proportion to the increase in CO2. The N2 concentration stays constant.
- Type 3 foul air occurs with the introduction of methane and nitrogen production and the non-respiratory uptake of O2 as well as CO2 stripping by water. Also falling into Halbert’s third type is an atmosphere which results from a combination of Types 1 & 2 with addition of another mechanism, which alters the gas concentrations.
Origin of the terms in speleology
James and Dyson (1981) were probably the first to document the terms “pink puffer and blue bloater” in a speleological sense. They reported observing the responses of two types of individual exposed to foul air containing a high concentration of CO2. Most cavers respond by hyperventilating and with some degree of blood vessel dilation near the skin, which results in a pinkish complexion. Dubbed the pink puffers, this description fits the overwhelming majority of cavers. A very small minority have a greatly reduced response to high CO2. Because they do not hyperventilate their oxygen level in the lungs and blood is reduced, thus giving a slight bluish tinge to their skin. Dubbed the Blue Bloaters, these people have a greatly increased chance of passing out. Therefore “a known blue bloater should never enter a region of CO2 without the warning companionship of a pink puffer” (James and Dyson 1981).
James and Dyson used these terms in the speleological arena because the outward physiological effect on cavers exposed to foul air often matched those of medical patients suffering COAD. The terms, pink puffer and blue bloater, were certainly in use by anaesthetists and respiratorists for some time prior to the publishing of James and Dyson’s 1981 paper. For example, an article titled “Blue Bloater: Pink Puffer” was published in the British Medical Journal in 1968 and refers to the terms first being used around 1958. (Anon 1968).
Foul air effects on humans
To understand why cavers can be categorised as either a pink puffers or blue bloaters, one must look more closely at the physiological effects on a person exposed to foul air of varying CO2 and O2 concentrations. Indications are that a person’s degree of reaction to foul air, is closely linked to the gas which is their primary regulator of breathing and heart rate. Bearing in mind that “a high CO2 concentration is the most life threatening situation encountered underground while a life threatening low O2 concentration is rarely encountered” (Smith, 1999b). Hence the warning by James and Dyson (1981), that a blue bloater should never enter a region of CO2 without the warning companionship of a pink puffer needs to be reinforced.
Our respiratory system needs to work harder for us to cope with foul air. The red cell haemoglobin in our blood, transports O2 and CO2 between the lung and body cells by the blood circulation. The exchange of the two gases takes place in the lungs by diffusion across the walls of the air sacs (alveoli). Oxygen from inspired air diffuses across the lining of the air sacs and enters the blood, while CO2 moves in the opposite direction. Diffusion occurs because a gas in high concentration will move to an area of relatively low concentration, until an equilibrium is reached. Breathing in foul air with an elevated CO2, reduces the ability of the body to get rid of its waste CO2 to the exhaled air. This causes an elevated CO2 concentration in the blood, resulting in acidemia, in which the body tries to counteract by initiating a number of secondary mechanisms in an attempt to return the pH toward normal (Smith 1997a,b).
In simplified terms, if the inhaled foul air contains a relatively high concentration of CO2 the haemoglobin is unable to get rid of the body’s waste CO2, thus the haemoglobin is not free to take on fresh O2. Exposure to a high concentration of CO2 can result in respiratory acidosis, coma, asphyxiation and death.
Pink puffers from a speleo perspective
Most cavers react quickly by hyperventilating, when exposed to foul air containing an elevated CO2 concentration. They also take on a pinkish complexion due to some degree of blood vessel dilation (cutaneous vasodilatation) near the skin. Other symptoms include headaches, clumsiness, fatigue, anxiety and loss of energy. Amongst the speleological fraternity these people are colloquially known as “pink puffers”.
This reaction is considered “normal” amongst the human population and can be explained by a well known medical fact that most humans rely on CO2 as their body’s primary trigger to regulate breathing and heart rate. Nerve receptors in the aorta near the heart and in the carotid artery, which goes to the brain, monitor any rise in blood CO2 and the brain’s control centre reacts by accelerating the breathing and heart rates. In effect the body is trying to reduce the blood CO2 and take in more O2 through gas exchange in the lungs. Changes in blood O2 are also monitored, but the receptors are not as sensitive to changes in O2 as to CO2. Hence the secondary trigger for regulating breathing and heart function is a lack of O2 which is detected by sensors in the carotid arteries and aorta arch lining near the heart.
Blue bloaters from a speleo’s perspective
Blue bloaters, on the other hand, do not respond to elevated concentrations of CO2 as quickly as pink puffers. By not hyperventilating, the oxygen level in their lungs and blood is reduced. This causes cyanosis (reduced O2 in blood), thus giving a slight bluish tinge to their skin. These people have a greatly increased chance of losing consciousness without warning.
It is medically recognised, that for a small percentage of the human population, their primary trigger for regulating breathing and heart rates, is reduced O2 in the blood.
Medical references to pink puffer and blue bloater
Doctors and scientists have written many research papers on the subject of Chronic Obstructive Airways Disease (COAD) which over time has been known by a number of other names, including Chronic Obstructive Pulmonary Disease (COPD), Chronic Airflow Limitation (CAL), Chronic Airways Disease (CAD) and Obstructive Airways Disease (OAD)
Medical patients with COAD clinically cover a wide spectrum and those extremes have become known as pink puffers and blue bloaters. Two components of COAD are emphysema1 and chronic bronchitis2. When these diseases are examined in their relatively pure form, each has its own striking patient characteristics of body build, general appearance and underlying disordered physiologic condition. That is, pink puffers are emphysema patients and blue bloaters are chronic bronchitis patients (Mandavia and Dailey 1993). However, Voelkel (2000) stresses that “while COPD patients are viewed traditionally as being either blue bloaters or pink puffers, guidelines have made efforts to stress that many patients will fall into neither group”.
Medical papers often quote significantly different figures as to the proportion of COAD sufferers in a given population. For example, Duffy (2000) quotes about 5% of the United States population are COAD sufferers, while Hunter et al (2001) quote approximately 20%. Mandavia and Dailey (1993) quote COPD as effecting more than 25% of all adults in the USA. These vastly different figures reflect the conflicts of definition between doctors and authorities.
Pink puffers and blue bloaters from a medical perspective
Pink puffers are patients with COPD where the pathology is widespread emphysema1. Their main symptom is breathlessness which is progressive, because their blood gases are relatively normal, their skin is of good colour and in the case of Caucasians, has a pink colour. They are of thin build and have evidence of airways obstruction with a reduced exhaling capacity - forced expired volume in one second (FEV1). Their chests are over inflated (hyperinflated) due to air trapping and the diffusing capacity of the lungs for carbon monoxide (DLco)3 is reduced. A disease of the heart (cor pulmonale)4 is unusual and when it occurs is usually late in the disease. (West 1977, DeMarco et al 1981).
On the other hand, blue bloaters have mostly a severe bronchitis2 with some emphysema1. They are overweight and have a chronic cough with sputum (sometimes purulent). They have an elevated carbon dioxide and low oxygen in the blood. There is severe airway obstruction with a reduced FEV1. Lung volumes and DLco may be normal. The patients have a plethoric5 appearance due to polycythaemia (an increase in the number of red cells due to chronic hypoxia6), and are cyanosed (blue) because of low blood oxygen. Chronic hypoxia causes the pulmonary blood vessels in these patients to constrict so that the right side of the heart has to pump much harder. This is worsened by the thickening of the blood (polycythaemia) and leads to thickening of the muscle in the right side of the heart (cor pulmonale) with subsequent failure and fluid retention. These changes occur relatively early in the disease and give the blue bloater appearance. Patients usually respond very well to correcting the hypoxia with long term oxygen therapy (West 1977).
|
Figure 1. Blue Bloater - chronic bronchitis. |
Figure 2. Pink Puffer – emphysema |
| Figures 1 & 2. Reproduced from a paper titled ‘Chronic Obstructive Pulmonary Disease’ by Mandavia and Dailey (1993) | |
Validity of these terms in today’s medical profession
The outward appearance of the patient is an interesting aspect to scrutinise. Certainly the subtle difference in skin colour (pink), may be true for persons of white Caucasian background, but would be less discernible for persons of dark coloured skin. If we just consider this aspect, one could speculate that the terms originated from within the Caucasian medical profession.
The “Puffer” term certainly refers to the fact that the patient is hyperventilating. The “Bloater” term may be interpreted as being swollen or enlarged and is referring to the physical appearance (obesity) of the patient.
The medical profession has traditionally viewed patients with COAD as being either blue bloaters or pink puffers, however more recent guidelines stress that most patients will not fall into either category. The COAD medical condition now covers such a wide spectrum in relation to the traditional terms which only describes patients at the extremes of COAD.
Given that today’s society is more attuned to acceptance of a mixed ethnic population and the use of a political correct vocabulary, the medical fraternity is moving away from these terms to categorise COAD patients.
What exactly is COAD?
Howard (1990) gives the following definition:
Chronic irreversible obstructive airways disease is the end result of a number of disorders: airway damage from tobacco smoke, atmospheric pollution and occupational dust and fume, bronchiectasis, cystic fibrosis, bronchial asthma7 and a number of congenital disorders of defective airway defence. The clinical features include sputum, wheezing, breathlessness and infective and noninfective airway inflammation8. The pathological consequences are airways obstruction, emphysema and respiratory failure.
Duffy (2000) states: In clinical practice most emergency physicians use the term more specifically for the conditions of emphysema and chronic bronchitis, tending to view patients with conditions such as asthma7, bronchiectasis and cystic fibrosis as different entities, even though the clinical margins are often blurred and treatment options often overlap considerably
In general, medical authorities now use the term COAD to cover all chronic respiratory conditions in which a person has irreversible reduced expiratory airflow. Some medical references also include asthma in the definition of COAD, even though asthma is a reversible airway obstruction.
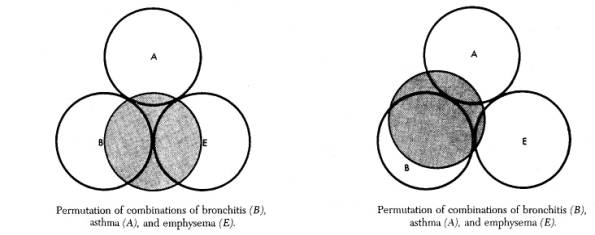 |
| Diagram by Mandavia and Dailey (1993) which shows that a combination of several illnesses (of varying degrees) may contribute to a patients COAD condition. The shaded circle represents the individual patient |
An exacerbation9 can be diagnosed if an increase in breathlessness and/or an increase in sputum are experienced for two or more consecutive days. Other symptoms may include wheezing, sore throat, fever and cough (Thiadens et al 1998).
Voelkel (2000) says it is a commonly perceived myth that COPD is solely a self-inflicted disease of elderly smokers. He highlights that while smoking is a major risk factor for developing COPD, it is not the only cause and a sufferer may not be elderly.
A study undertaken by the Primary Healthcare Centre in the Netherlands (Thiadens et al 1998), cited years of smoking as the major contributor to COPD conditions. Their study of 192 patients aged 18-75 years, who presented themselves to their general practitioner with a cough persisting for at least2 weeks, concluded:
About half ……….. have asthma7 or chronicobstructive pulmonary disease. With a simple formula based onthree symptoms and prolonged expiration, pack years of smoking10,and female sex, most patients may be identified correctly in generalpractice (Thiadens et al 1998).
It is well established that cigarette smoking is the major risk factor with an estimated 10 to 30% developing COPD, however many smokers may not develop clinically significant airflow limitation. Owing to the large pulmonary function reserve, airflow obstructions can progress undetected for many years without the development of overt clinical symptoms of disease. Thus while many patients diagnosed with COPD are elderly, a decline in lung function often can be detected in smokers as young as 40 years of age. COPD is an indolent disease process that only produces symptoms when a considerable loss of the lung function has occurred (Voelkel 2000).
Mulloy et al (1996) studied 19 severe COPD patients and found that the majority desaturated during treadmill exercise, with a fall of greater than 5% saturation of arterial oxygen (SaO2) and that the SaO2 fell twice as much during sleep as during maximal exercise.
Thiadens et al (1998) studied 192 patients who presented to their general medical practice with a persistent cough over two weeks prior to the consultation. Of these 74 were diagnosed with asthma and 14 with COPD.
Breathlessness is of variable severity when the Forced Expiratory Volume (FEV1) falls below 1.0 litre per second resulting in disability ranging from manageable to severe.(Howard 1990)
Breathlessness is a common feature of acute infective exacerbations, but breathlessness during normal every day activity develops insidiously over many years and most patients will have lost more than 50% of their predicted FEV1 by the time that breathlessness becomes a problem. (Voelkel 2000)
Comparing medical pink puffers with blue bloaters
Weight loss is common in patients with long standing disease with predominately emphysema (the Pink Puffer), although weight gain may also be a feature suggesting chronic hypoxemia11 and the onset of cor pulmonale4 (the Blue Bloater).
Johnson et al (1983) say that:
Pink and puffing patients (fighters) are frequently stated to maintain relatively normal blood gas tensions at the expense of breathlessness and are consequently severely disabled, whereas blue and bloated patients (non-fighters) choose to be free of breathlessness and are less disabled, but at the expense of abnormal blood gas tensions and consequent right heart failure (right ventricle failure).
They studied 26 patients (15 pink puffers and 11 blue bloaters) with chronic airflow limitation (with closely matched spirometric values12) to see if the fight to maintain normal blood gases had a noticeable cost in terms of increased disability. Measurements were made of the breathlessness, exercise tolerance, and exercise physiology of the two groups. They found that blue bloaters “chose” to tolerate abnormal blood gas tensions, as they were able to improve the pressure of arterial oxygen (PaO2) and pressure of arterial carbon dioxide (PaCO2) considerably toward normal by voluntary hyperventilation. They failed to find any difference in breathlessness or exercise tolerance between the two groups despite a higher ventilatory response to exercise in the pink puffers. They conclude:
The misconception that the pink puffer patients are more breathless may have arisen from the increased ventilatory response to exercise, so that patients are seen to puff and thus look breathless. It may also reflect differences in way of life, with the pink puffer playing the hare, always rushing at life, in contrast with the tortoise blue bloater, who plods at one pace and never becomes breathless (Johnson et al 1983).
A possible link between smokers and speleological blue bloaters
A few quotes are used here to outline COAD and its links with smoking
Voelkel (2000) states: “smoking is a major risk factor for developing COPD.
Kerstjens (1999), states: “Chronic obstructive pulmonary disease is largely preventable. The main cause is exposure to cigarette smoke. Thedisease is rare in lifetime non-smokers.”
Voelkel (2000) comments that: “many smokers may not develop clinically significant airflow limitation…….. Owing to the large pulmonary function reserve, airflow obstructions can progress undetected for many years without the development of overt clinical symptoms of disease.”
Thiadens et al (1998) highlights that: “In the early stages of COPD, patients may only experience mild breathlessness when taking exercise, but older patients are often at the stage of their disease where they are unable to care for themselves because they are too short of breath.”
Bear in mind that, COAD sufferers could actually be chronic asthma or bronchitis sufferers, which may or may not be linked to smoking.
Over the past 30 years the author has been into many caves containing foul air and observed the reactions of fellow cavers. What particularly stood out were the reactions of smokers and non-smokers when foul air was first encountered. These informal observations indicated that a higher percentage of heavy smokers react slowly to elevated concentrations of CO2 compared to non-smokers. At a cursory glance it would appear that many long term, heavy smokers could fit into the category of blue bloaters. Ex-smokers could be either pink puffers or blue bloaters. One could speculate that this may be due to a person’s history of physiological conditions, which resulted in prolonged restriction of lung or respiratory function. Thus their body has become acclimatized to elevated CO2 in the lungs and blood. This condition may have reverted their primary trigger to an O2 deficiency and now uses the body’s CO2 sensors, as the secondary trigger to control breathing and heart rates.
Discussion
Two possible scenarios are put forward for discussion.
1. Given that speleology is a physical sport and a reasonable degree of fitness is required to go caving, one could speculate that in speleological terms, a high proportion of blue bloaters may well be people with COAD at a stage, which is undiagnosed. Given that this disease progresses undetected for a long time before it impacts on the physical life of a person, it may have inverted the persons main trigger for their breathing function. Hence they may not respond as quickly to elevated CO2, in a cave atmosphere as non-COAD cavers and as such have a greatly increased chance of losing consciousness without warning.
Lippmann (1992) appears to support this scenario by stating:
Some people have chronic obstructive airways disease, such as chronic bronchitis or emphysema which may cause excess carbon dioxide to be trapped in the airways. Certain sufferers become less sensitive to carbon dioxide to stimulate their breathing and rely more than normal on diminishing blood oxygen levels to cause them to breathe.
Little evidence could be found amongst other medical literature to suggest that the onset of COAD may have reverted a person’s primary trigger to an O2 deficiency and use the body’s CO2 sensors, as the secondary trigger to control breathing and heart rates.
2. A more accepted view in the medical fraternity is that patients who are going to become pink puffers or blue bloaters, medically speaking, were probably destined to become one or the other at birth. The mechanism which determines this is not fully understood. Blue bloaters have a dulled respiratory centre and respond less to a rise in CO2 concentration. Some 20% of the population have a pulmonary vascular bed which responds to hypoxia6 by vasoconstriction13 which causes hypertension14 in the pulmonary circulation, overloads the right heart which hypertrophies15 and subsequently fails causing swelling of the lower body. People with this basic physiological predisposition will probably develop blue bloater type COAD if they smoke heavily. Could it be that cavers who are speleological blue bloaters are probably destined to become medical blue bloaters later if they smoke heavily and develop COAD?
Certainly these two scenarios could form the basis of a research project for someone with access to equipment, capable of lung function measurements over a diverse range of individuals. Another consideration would be the large variation in levels of fitness amongst cavers – both smokers and non smokers.
Conclusion
The terms pink puffers and blue bloaters are used by speleologists in a colloquial sense to categorise how individuals react when breathing foul air in caves. Pink puffers hyperventilate and have good colour, while blue bloaters react slowly and look bluish because they are starved of oxygen. In foul air, a blue bloater runs the risk of losing consciousness without warning. James and Dyson’s (1981) were quite within reason when they associated the medical term to describe the physiological effect of foul air on cavers. However, while the subtle difference in skin colour may be true for persons of white Caucasian background, it is less discernible with persons of darker coloured skin.
Amongst the medical profession, patients with Chronic Obstructive Airways Disease (COAD) were traditionally viewed as being either “blue bloaters” or “pink puffers” because the terms described their outward appearance and reaction to breathing good air. More recent guidelines stress that most COAD patients won’t fall into either group because the medical condition covers such a wide spectrum. The traditional terms pink puffer and blue bloater, were only describing patients at the extremes of COAD. The terms were used by the medical profession, to characterise the patient’s general skin colour, body build and breathing habits in good air. Now the terms are rarely used by the medical fraternity, particularly with the awareness of the need for a politically correct vocabulary.
Over the past 30 years the author has observed the reactions of fellow cavers to foul air. At a cursory glance it would appear many long term, heavy smokers fit into the category of blue bloaters. Ex-smokers are either pink puffers or blue bloaters, and the majority of non smokers being pink puffers. Could this apparent high average of blue bloaters among smokers be due to their body becoming acclimatized to elevated CO2 in the lungs and blood, thus reverting their primary trigger to an O2 deficiency to control breathing and heart rates?
Two possible scenarios are put forward for discussion, which could link speleology blue bloaters, with smoking and the early stages of COAD.
1. Do long term smokers have an increased chance of being a speleological blue bloater because the early stages of COAD may have reverted their primary trigger to an O2 deficiency and use the body’s CO2 sensors, as the secondary trigger to control breathing and heart rate?
2. Is a persons destiny as a speleological pink puffers or blue bloaters, determined at birth well before the influence of smoking or COAD? At birth approximately 20% of the population have a pulmonary vascular bed which responds to hypoxia by vasoconstriction13. People with this basic physiological predisposition are more likely to develop medical blue bloater type COAD if they smoke heavily. Is it an early sign that a speleological blue bloater will become a medical blue bloater if they smoke heavily and develop COAD?
These two scenarios could certainly form the basis of a research project for someone with access to equipment, capable of lung function measurements over a diverse range of individuals.
Acknowledgement
I would especially like to thank Andy Spate for critically reviewing this paper.
Also considered while writing this paper were helpful comments via email from Dr. John West, Professor of Medicine and Physiology, School of Medicine, University of California, San Diego and valued comments from other respiratory specialists.
Footnotes
1. Emphysema is an abnormal permanentenlargement of the air spaces distal to the terminal bronchioles,accompanied by destruction of their walls and without obviousfibrosis (Kerstjens 1999).
In emphysema the walls of the tiny air sacs (alveoli) within the lungs are gradually destroyed. The lungs lose elasticity and can no longer expand and contract easily to draw in and force out air. The disease develops so slowly that its victims are generally unaware that anything serious is wrong until much of the lung function in impaired (Howard and Lewis 1986).
2. Chronic bronchitis is defined as chronic cough, mucusproduction, or both, for at least three months for at least twosuccessive years where other causes of chronic cough have beenexcluded (Kerstjens 1999). Bronchitis usually results from a viral infection, such as a cold, which spreads down into the bronchi and is followed by a bacterial infection.
3.A measurement of the diffusion capacity for carbon monoxide (DLco) directly reflects the integrity of the alveolar capillary unit, and is useful for separating emphysema from the other forms of COPD, particularly in patients without substantial clinical signs. (Buist et al 1991)
4.Cor pulmonale: disease of the heart characterized by hypertrophy and dilatation of the right ventricle and secondary to disease of the lungs or their blood vessels.
5.Plethoric is a bodily condition characterized by an excess of blood and marked by turgescence (swollen or inflamed) and a reddish complexion.
6.Hypoxia is a deficiency of oxygen reaching the tissues of the body.
7.Chronic Asthma is a condition characterised by frequent bouts of breathlessness. In an asthma attack, the bronchi become narrow because their walls contract and cause partial obstruction of the airway, which makes breathing difficult. The mucous membrane lining may swell and be accompanied be secretion of thick sticky mucus. An attack may be brought on by an allergic reaction to airborne particles, such as:- pollen, mould spores, dust and animal fur (The Family Medical Reference Book. 1987). Some medical references also include asthma in the definition of COAD, even though asthma is a reversible airway obstruction.
8.Airway inflammation is an inflammation of the airway which restricts airflow to the lungs.
9.Exacerbation: to aggravate or make a medical condition more severe.
10.Pack years of smoking were calculated as the product of years of smoking and the mean number of cigarettes per day divided by 20.
11.Hypoxemia: deficient oxygenation of the blood; condition of having less than normal oxygen in the blood.
12.Spirometric values: are measurements made to determine the efficiency or the respiratory system. eg. FEV1: Forced expired volume in one second.
13.Vasoconstriction:contraction of the muscular coat in the wall of arteries, which reduces the blood vessel bore and the amount of blood flow.
14.Hypertension: abnormally high blood pressure and especially arterial blood pressure.
15.Hypertrophies: Excessive development, morbid enlargement of an organ.
Bibliography and References.
Anon, 1968 Blue Bloater: Pink Puffer, British Medical Journal. 2(606): 677
Buist, A.S., Petty, T.L., Wiedemann, H.P., 1991 COPD: don’t wait until it’s obvious, (diagnosing chronic obstructive pulmonary disease), Patient Care, 25(20): 60-74
DeMarco, F. J., Wynne, J.W., Block, A.J., Boysen, P.G., Taasan, V.C., 1981 Oxygen Desaturation During Sleep as a Determinant of the “Blue and Bloated” Syndrome. CHEST, 79(6): 621-625
Duffy, M., 2000 Chronic Obstructive Airways Disease, Textbook Of Adult Emergency Medicine. Chapter 5.4, pp. 216- 220. Harcourt Publishers Ltd, London
Halbert, E.J.M., 1982 Evaluation of Carbon Dioxide and Oxygen data in atmospheres using the Gibbs Triangle and Cave Air Index. Helictite, 20(2): 60-68, Journal of Australasian Cave Research.
Howard, P., 1990 Natural History of Obstructive Airways Disease and Hypoxia: Implications for Therapy. Lung , Supplement, pp. 743-750.
Howard, R and Lewis M.E., 1986 Emphysema, The people’s Medical Manual, pp 216-217
Hunter, M.H., and King D.E., 2001 COPD: Management of Acute Exacerbation and Chronic Stable Disease. American Family Physician, 64(i4): 603
James. J. and Dyson, J., 1981 Cave Science Topics: CO2 in Caves, Caving International, 13: 54-59
Johnson, M.A., Woodcock, A.A., Rehahn, M., Geddes, D.M., 1983 Are ‘pink puffers’ more breathless than ‘blue bloaters’?. British Medical Journal – Clinical Research Ed. 286: pp. 179-182
Kerstjens, H.A.M., 1999 Stable Chronic Obstructive Pulmonary Disease, British Medical Journal, 319: 495-500
Lippmann, J. 1992 Adverse Reaction to Oxygen, Chapter 5, pp. 59–61, Oxygen First Aid, Published by J.L Publications, a Division of Submariner Publications Pty Ltd. P.O Box 387, Ashburton, Victoria 3147, Australia.
Mandavia, D.P, and Dailey R. H., 1993 Chronic Obstructive Pulmonary Disease, Chapter 96, pp. 1494-1511, Emergency Medicine – Concepts and Clinical Practice, Fourth Edition 1998.
Mulloy, E and McNicholas, W.T., 1996 Ventilation and gas exchange during sleep and exercise in severe COPD. CHEST, Feb 1996, 109(2): 387-394
Smith, G.K, 1997a Naked Flame Tests for CO2 in Limestone Caves & The Effect of CO2 and O2 on Humans, pp. 40-52, Proceedings of the 21st Biennial Conference of the Australian Speleological Federation Inc.
Smith, G.K, 1997b Caves, Carbon Dioxide & You. Australian Speleological Federation Inc. pp. 35-39, Proceedings of the 21st Biennial Conference,. Updated from the original article publication in 1993, Australian Caver, 133: 20-23
Smith, G.K, 1997c Unseen Danger Of Foul Air & The Flame Test. Australian Caver. 141: 13-16
Smith, G.K, 1999a Glossary Of Caving Terms. Caving Queensland: Australian Speleological Federation’s, pp. 61-83, 22nd Biennial Conference Proceedings 1999.
Smith, G.K, 1999b Foul Air In Limestone Caves And Its Effect On Cavers. Caving Queensland: Australian Speleological Federation’s, pp. 48-58, 22nd Biennial Conference Proceedings 1999.
The Family Medical Reference Book 1987 The Respiratory System, pp. 84 – 99. Macdonald & Co. (Publishers) Ltd. 66-73 Shoe Lane, London
Thiadens, H.A., 1998 Identifying asthma and chronic obstructive pulmonary disease in patients with persistent cough presenting to general practitioners: descriptive study, British Medical Journal, 316: 1286-1290 (25April).
Voelkel, N.F, 2000 Raising Awareness of COPD in Primary Care. CHEST, 117(5), Supplement. pp. 372S–375S. COPD; Working Towards A Greater Understanding.
West, J.B, 1977 Pulmonary Pathophysiology – The Essentials. Baltimore: Williams and Wilkins Co.
Comments are most welcome.





